|
Okay, So Mom has been admitted yet again to the local hospital. 'Visit Mom', your android app calendar chimes. You groan and put your right indicator to the hospital. You find the parking space and the ward half an hour later. So how is mum? you ask the nurse with the not-so-well-ironed-shirt. "I am only a bank nurse. The staff nurse in charge is on a break". You don't dare ask the duration of the break lest you infringe the human rights agreement with other countries including Brussels. You wait. Mom is sleeping. You don't dare wake her up lest she starts ranting again. You don't even know when she started getting her dementia because you thought she always used to rant anyway. The nurse breaks your reverie. "Can i help you" " I am my mom's son"- you cringe hearing yourself and continue anyway- "Are there any plans to get her home yet?". A well practised shrug and a helpless grimace tells you everything you need to know. "We are waiting for the therapy report and then the social worker will have to liaise with her GP regarding funding issues depending on which I will put out the section XXIII form which will then trigger the community social worker to talk to her carer agency who will then......." You are not sure what you just heard but you nod anyway because that shows you have been brought up in a civilised family. "Any idea about time scales?" You don't know why you sounded like a browbeaten loser but you sounded like that. "We will let you know when we hear something. Just ask one of the nurses when you come next time"...and the next time and the next time...You wonder if the room has an echo. The nurse leaves and you decide to leave quietly, having done your bit as the "good son". "Is that you Patrick?"...oh no Mom, you need to go back to sleep. I am in a hurry. You make the heart wrenching decision to sit down anyway and hold her hand. You see the daily newspaper on mom's lap. The headline news thankfully is not yet another terrorist bombing but instead about bed blockers in the NHS delaying timely care to many others. Mom made it to the national news. Finally!
0 Comments
Disclaimer:
The statements below do not reflect my practice, my biases or my decision making process. There is no intention to trivialise the issue, but there is an intent to attempt at frivolity All of us want to make the right decision. But let us not kid ourselves; the recent issue about the DNAR generated by the court order (court document: / uk resus council guidance) is not about making the right decision or giving the right treatment for the right patient, but instead about being seen as making some decision, being seen as having some discussion and ultimately documenting something so that it stands up in court if or when a relative escalates the issue. Forget the actual decision, forget the decision making process, forget documenting; we are having trouble just getting discussions started in 93 year old stone-deaf people, the 50 year old bed-bound woman with severely disabling multiple sclerosis and the 40 year old with advanced alcoholic cirrhosis with an off- the -scale Child-Pugh score on his usual admission yet again this year. We now need a trigger to start discussions off in everyone admitted through the hospital doors to meet legal requirements. Solutions are popping up everywhere to help patients in hospital beds to engage with their own death-bed scenarios. A leaflet? A poster? An overhead TV screensaver reading "DNAR- Now available to everyone on the NHS"? A local radio station DJ singing “Ask about D-NAR” along Y-MCA lines? A badge on the beautiful nurse which reads “ it is ok to ask about DNAR” (while you ask about my hand-washing skills)? An offer of patient choice of hospital gowns with "FOR" or "NOT FOR" printed in fluorescent yellow? I am full of ideas today I am. So we have concerns about inclusion as well as exclusion. With regards to inclusion: The court states: "If the clinician forms the view that a patient will not suffer harm if they are consulted, the fact that they may find the topic distressing is unlikely to make it inappropriate to involve them.” The court has in effect stated that patient's emotional distress is not harm?. Or maybe, the court has stated that the potential to cause emotional distress is not harm. So, in effect we are left with having to start discussions with people who we know are very likely to be emotionally distressed by the discussion, often pointlessly, and then stop half-way when we find them in emotional distress and leave them wondering what would have been had the conversation been completed…?? With regards to exclusion: “The distress must be likely to cause the patient a degree of harm to warrant them not having the decision discussed with or explained to them." I am keen to avoid emotional distress to my patients when they are most vulnerable. I am keen to write in many instances that I feel that it would not be appropriate to discuss the issue of CPR with this patient in front of me. But how do I document the perception of a degree of "emotional distress" that can equate to "legal harm"? Apparently we are not supposed to be concerned about our own distress with all of this as human beings, but apparently the court expects every one of us when we qualify as doctors suddenly to be efficient DNAR machines, moving from patient to patient, discussing heartlessly yet empathetically, rapidly yet effectively, legally yet ridiculously. In a setting in the near future, where I refuse to discuss DNAR with a patient(s) due to my concern about it potentially causing significant distress to both me and the patient, I think it would be helpful if we had a few doctors available at hand who have been on courses and returned as "DNAR officers" who have the authority to identify "legally acceptable patient distress", who then goes around with a fixed state of mind on "DNAR rounds" perhaps, to ensure everyone is treated equally? It would be even better if these DNAR officers were lawyers or judges who can make better decisions since they are apparently well qualified to make decisions about decisions that they never have to make themselves. A DNAR discussion in the community can make our job easier in some cases(if they have chosen against CPR) , and more difficult in many cases( if they have chosen pro-CPR), but no less in terms of numbers, as everyone will still need to have had a discussion with at admission to hospital.. So, what can be done to engage patients in the issue of their own potential for mortality during an otherwise seemingly innocuous hospital admission? “if a clinician considers that CPR will not work the patient cannot require him/her to provide CPR. It states that this does not, however, mean that the patient is not entitled to know that the clinical decision has been taken.” We all agree that the patient is entitled to know it. But we would like some patients to initiate the conversation though. So, then, should a leaflet at admission merely highlight this entitlement perhaps, with a generic approach including, welcome to the ward…., the ward facilities are….and by the way you are entitled to look at your drug charts, monitoring charts and particularly case notes if you would like to know or discuss about your DNAR status. If the patient does not read or reads but does not discuss, doctors still stand the risk of going to court. So, going one step further, the leaflet handed over to clients entering the hospital premises could have a tear off section with tick box options: 1. I want to discuss my resuscitation status every time I get admitted. 2. I do not want to discuss my resuscitation status but want my relatives to have the discussion on my behalf (although the ultimate decision will be the doctors’ 3. I do not want to discuss my resuscitation status and I am happy for the doctors to make the DNAR decision on my behalf depending on my suitability for the treatment. 4. I do not want to be resuscitated. I do not want to discuss this further. Ever. Notably, there should never be the option 5: I want to be resuscitated. That would always be a patient's wish list and a doctor's decision. Thankfully that is not in question this year. Not yet. I remain grateful to the authors of the BMJ article for highlighting this “pain in the backside” that has been troubling me for the past few years. They rightly mention that Stage III CKD may not be all that it sounds like. It was music to my ears.
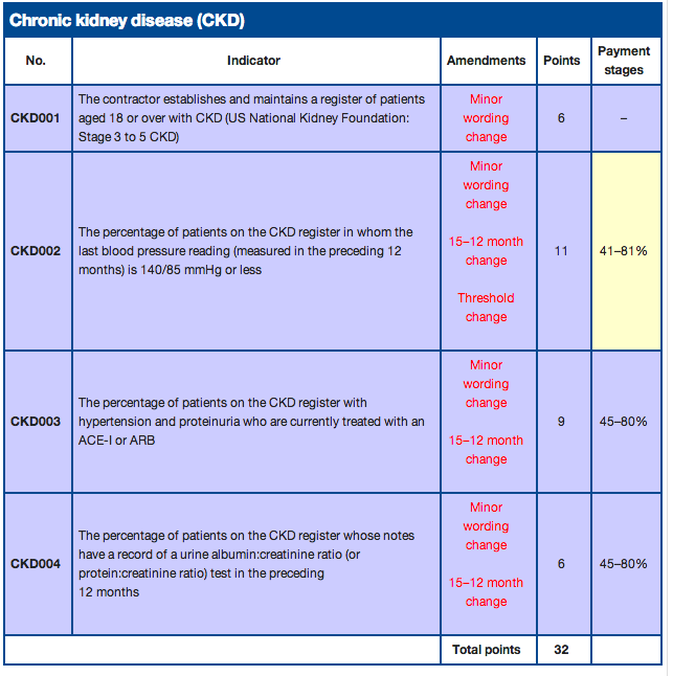
The changeover from Acute renal failure to AKI and Chronic renal failure to CKD happened slowly, but felt like an overnight attempt for many of the older generation accustomed to the older terminology. Change for change's sake was not the concern; instead, change that increased confusion with diversion of resources to a bogeyman blown out of proportion, was the main reason for annoyance for many. The new generation of practitioners who adore protocols, pathways and guidelines, love one another thing. Scores. Scoring everything makes life much easier. Whether it is a decision on who can go home to who will die in 24 hours. Live and die by the score. How then could the ease of five different stages of diagnosis based on another easy-to-do measurement not tickle the fancy of the vast majority? Without doubt it did. Subdivisions of some of the stages with added alphabets gave diagnoses a more authentic feeling. Discharge summaries never looked so good. Clinic letters carried more weight with those alphabets on. CKDIIIbp. Impressive. Communication at its best. LOL, TTYL. CKDIV. It all fitted in. Various organisations, full to the brim with think-tanks, have been sitting around tables on their aching bottoms, trying to decide whether 2 is same as 3, or is 3 as bad as 4. Was 3a worse than 3b or was it 3ap that was the troublemaker? By this stage, only a select few maintained interest in the nitty gritty of it. The rest of the world of generalists waited eagerly for the final decisions to be made so that they could continue with their work; work that mostly involved hunting for those individuals with the appropriate stages, so that they could be called by their true name, complete with suffixes! Why was that important? Because it was important to get the diagnosis right. Why was it important to get the diagnosis right? Because it was a disease. Which meant, that there would be performance indicators on how we, the good people in the NHS, manage the disease. If the complex scoring did not appeal to your senses, the QOF monies probably would. (see picture below) But those skeptics out there ( a dwindling resource, just like the witches of bygone era) despite fear of the stake, started speaking out in their own small realms about how the early stages of chronic kidney changes (CKC?) was a measurement sold as a diagnosis. Just like cholesterol perhaps. Just like IFG and IGT perhaps. Just like an osteopenic DEXA scan report. Just like a lowish testosterone in the ageing gentleman. But these days who is to complain? After all, we live in a world where obesity is a disease! The crusaders for the new definitions chanted that unless something was labelled as a disease, no one would take interest in screening for it, so as to identify it early, so that a whole host of life-extending medications could be given out to outwardly healthy looking, not-a-care-in-the-world individuals who were enjoying their life just about till then. 94 year old Martha thought she was healthy. Little did she know that her risk for death in the next 10 years was close to 99%. But now, with the help of the new CKDIIIap diagnosis, she will be able to understand the relative risk for all-cause and cardiovascular mortality and take measures to reduce her risk for death in the next decade. She would also have understood that her neighbour Susan, who had CKDIII a (but no p) would be more blessed and live till 104 easily. Even if Martha didn’t understand it and didn't give two hoots about it, her new SHO-turned-GP who was au fait with CKD staging would care. He would embark on urgent screening for microalbuminuria, dipstick for haematuria, culture urine to rule out any infections, check for anaemia and hyperparathyroidism, and arrange an ultrasound scan of the kidneys at the local hospital (which is now 60 miles away because the local one was no good at identifying CKDIII and had to be closed). He wouldn’t stop there though. He has been told by the guideline that anything that moves with CKD diagnosis should get antihypertensive treatment to normalise blood pressure to pre-pubertal levels. Full dose ACE inhibitor, Aspirin and Statin to be collected from Lloyds pharmacy please. News of Granny breaking her leg due to a fall because of low blood pressure and admitted to hospital where she bled to death from a peptic ulcer was merely collateral damage. For the greater good. So that many other nonagenarian lives may be saved. After all, that is what doctors do. They save lives. Prevent death. Totally. Whenever kids get killed in the US by a psycho with a gun, the gun lobby comes out to say that it is the man who pulls the trigger that kills and not the gun. The gun was a harmless device apparently till the perpetrator decide to convert it into a deadly weapon by activating it. Whether it is diagnosing ACS using a troponin rise, or CKD using eGFR values, or DVT using D dimer, ultimately it is a weapon that we offered to a psycho. The weapon was not a wrong thing totally, albeit a weapon but the real question is, do you want to give it to the psychos? Are responsible individuals interpreting the test and titrating investigations and treatment in an individualised manner? Who is to police, once the weapons have been dished out? Interestingly, guidelines state that CKDIII does not require referral to the specialist!!. So the psychos are now alone with a gun and told to seek help only if their urges get out of hand. I am not saying that all the new generation of doctors are psychos, just some of them So, what is the solution to all this confusion? Brave the jeers of "politically incorrect" and "double standards" and state that after 80 years of age, eGFRs may fall physiologically just like memory and muscle mass rather than pathologically in every instance, and adjust the nomograms to reflect that? Do we dare say that statement for fear of ageism? Do we bring back geriatrics as a speciality so that only a select few may think of the elderly differently and interpret eGFR in the right context and abide by primum non nocere? Or do we do the decent thing and select students who have the head screwed on right into medical schools and then try to teach them how to individualise care in every instance, how to use guidelines as a floodlight and not as a flashlight, and above all help them develop into true doctors who are happy to stand up and say, "not everybody requires treatment for everything measured"?? We know the NHS has many faults. Not enough staff at all levels, not enough continuity of care even when we have staff, poor handover of care, an error prone environment that cannot be made safer due to a multitude of reasons, suboptimal feedback to its workers on their performance, severe limitation in finances preventing investment to improve quality, so on and so forth. Amidst all that, we despair about the lack of compassion that patients experience while on the wards and seek to inject compassion into the work place through various mechanisms ranging from displacing trainees and employees from their workplace for a whole day or two for generic feel-good sessions, circulating documents stating that everyone needs to be compassionate from tomorrow, sending in teams of experienced wise old doctors and nurses to hospitals with poor statistics to identify instances of lack of compassion, to publishing bigger and bigger pdf documents reasserting that medical carers need to show compassion as a requirement of their job. I just wonder whether there may be some people who read those documents and think, "that is a good idea, I think I will from tomorrow!" or "damn it, I haven't been compassionate for the last year, time to turn a leaf!". I dont know and I never will know how some minds work, I suspect. But everyone who reads these documents and asserts others to do what it says because it sounds good seems to think that people do think like that?
When a patient with obesity comes to my clinic, only one thought goes through my mind. Does this person acknowledge the real problem? You may call it insight. I try not to, because you cannot diagnose or elicit insight as there is no objective test for it. In short, you can be played for a fool easily. Compassion, like insight, cannot be diagnosed with certainty to be present or absent merely based on an interview or a supervised clinical encounter. Much of the greatest shows of compassion happens behind curtains, as it always has. Would it be fair to say that true compassion is when you hold a patient's hand and look into his or her tearful eye and communicate to him without words that you feel his pain of his life being cut down in the prime, that you feel her fear of the unknown while the diagnosis is still pending, or acknowledge the loneliness that the loss of his wife has thrust him into for the rest of his existence? Now, what about the water jug that you pushed nearer to him? What about the TV that you switched back on after talking to him? What about stopping talking to one patient and going over to the patient with dementia at the other end of the ward to help him into his slippers? Are they acts of compassion? Or are they merely fulfilment of your duties as a healthcare professional, expected of you anyway merely because of your presence there? Are they merely a demonstration of your sensitivity to the patient's physical needs that you perceive are a requirement of a civilised society that we live in? Did you do them because if you didn't the patient or the other patients on the ward would have noticed it? Would you have felt bad for the rest of the day if you had not done those deeds when required of you? Or would you merely tell yourself, "not the end of the world" and move on to your bed time reading on Waldenstrom's macroglobulinaemia? I see people not fulfilling these small gestures of comfort everyday. I do not judge them because I cannot be sure if it is merely a lack of awareness of their surroundings that resulted in inaction on their part. Nor can I be sure whether they can't be bothered because it would only slow them down further from the things that really matter, the things that are really "counted" these days, starting with discharge summaries and ending with VTEs. Let us put compassion to the real test. A 25 year old girl with learning disabilities and minimal communication is admitted with vomiting, headache and skin rash. CT brain normal, A&E admits for ? meningitis having "done the needful" with ceftriaxone on flow. Medical SHO reclerks and desires a senior review for LP. Vague skin rash, glass test all done. CRP normal, mild leucopenia. No clinical signs of meningeal irritation. . Patient's father says, "I dont think she has meningitis, please don't do lumbar puncture on her" Registrar feels lumbar puncture is required. He also has heard somewhere that he has to act in the patient's best interests and not the father's best desire. He tells the father that the patient requires LP for medical reasons. LP attempted, fails. Anaesthetist called in, patient squirms, needs general anaesthetic for LP. Medical consultant comes in at this stage and says unlikely to be meningitis, no need for LP, stop antibiotics, go home. How do you as a reader feel all that went down? Was there a compassion issue here? Or was there only a medical experience issue? Was there only an issue of risk management or a pretest probability assessment? Was the consultant's decision the result of compassion informing knowledge or knowledge and experience influencing compassion? Do you think that the same registrar would make a different decision one year later when he becomes a consultant and has to deal with a similar case? Would he put his GMC number on the line for compassion despite the pervasive worry that this case could be meningitis although nothing else says it is? Is compassion being demonstrated when you make difficult decisions instead of the easy ones that would give you good sleep at the cost of bit of discomfort for the patient? Would every consultant have made that same decision? Do you the reader feel aghast that the consultant went out on a limb dangerously and is to be kept a close eye on for further failings? My point is, compassion extends beyond emotion and comfort. It is intricately hidden in many of our day to day clinical decisions. It cannot be measured because it is not evaluated for, specifically. Particularly by those who do not recognise it for what it is. Assuming that we have established that compassion comes in various shapes and forms, visibly and invisibly, let us ask the more difficult question. "What then, is it that makes some people compassionate?" Or is the real question "what is it that makes some people WANT to be compassionate?". The difference is more than merely whether you look at it from the point of view of the receiver of compassion versus the provider of it. What I am really trying to understand is whether a person who shows compassion is purely driven involuntarily and intuitively to show compassion because he or she does not know anything different versus someone who wants to show compassion because they feel that not to show it would be unacceptable as an option, to society or to people in the immediate visible vicinity. An occasional encounter or an assessment while being observed for the eportfolio or an artificial setting where everyone is on their relaxed best behaviour will not distinguish between the two drivers. On the other hand, a long term knowledge of the personality of the person and his or her interactions with other colleagues could provide us with an idea of which of the two drives his compassion. To split hairs further could remove the fun for those engaging superficially with this concept and hence I will leave it at that level for now. For those wanting some intellectual take on this, have a look at "compassionate care: the theory and the reality" Is a compassionate clinician more effective in today's and tomorrow's world of medical care? I would like to pursue that question further but I am aware of the increasing length of the blog. I haven't checked the current requirements for admission into medical school but I am fairly certain that being compassionate or being able to be compassionate is definitely not an essential requirement. After all, we can teach them how to be compassionate after spending 5 years in medical school can't we? If you believe that, you are likely to merely see sarcasm in what I write and nothing beyond. You may even be contemplating a school to convert terrorists to be ambassadors for their country. At the end of the day, the real question remains. "Can we make non-compassionate people compassionate?" Or more realistically, "is amplifying the compassionate feelings that lurk in the subconsciousness of good people, tuning it up to increased sensitivity and awareness, the best we can hope for?" So if we believe that compassion can be taught in medical school or acquired at the workplace over time, how are we making sure that it happens? When was the last time you thought at the end of a trainee's posting; "that trainee has become more compassionate over the past four months here"? These days there are very few opportunities for anyone to get a feel for anyone's compassion on a day to day basis. The amount of exposure to each other, whether nurse-doctor or trainee-supervisor is so minimal that generic skills are increasingly assumed to be present in people based on their interactions with you. How does a person / doctor behave when they have nothing to gain from the other person? When there is no fear of negative feedback? When there is no need to impress another? When there is no desire for reassurance from others? When showing compassion is more likely to slow you down in your work? When showing compassion is unlikely to be appreciated by anyone {imagine one to one with a dementia patient behind a curtain}? When showing compassion can put you at risk of censure? {see case example above}. In one sentence, true compassion cannot be assessed, because you are never there when it happens. We just live in hope that we have the right people in the right jobs. When we start suspecting the absence of true compassion, we will convert hospitals and nursing homes into big brother houses to enforce compassion. The problem is, we convert a fine human sentiment into a duty of care that takes away the pride that good people get from its delivery. There is no going back if that happens. So the people living near MidStaffs are now showing their anger at plans for A&E closure at their local hospital.
What does that tell us? Does it tell us that they now feel that the local hospital is safe? Does it tell us that they are willing to forget the "atrocities" attributed-rightly or wrongly- to that hospital over the past 7 years? Does it mean that they think that the hospital was wrongly blamed in the past and the sins were exaggerated to the point of unwarranted closure? Or does it merely tell us that a hospital closure is what it takes these days to get the local community to speak up for that hospital? Sadly, that is human behaviour of the masses. We will always wonder why the Jews did not fight against the visible practices that none of them agreed with. We will always wonder when the perfect time is to use a nuclear device against aggression; when the hostiles are at Calais? or Midway across the channel? or at Dover? When is it really time for appropriate and timely aggression? Before the internet and widespread television, people believed that Elvis was still alive somewhere. Maybe not in the building, but somewhere. The same would have been true for Michael Jackson as well if we did not have the media telling us the truth all the time that he was dead and wouldn't be coming back. So when do we stop believing what we hear or see in the media that we rely on so much to keep ourselves informed? Or more importantly, what makes us choose to believe or not to believe what we read in the news everyday? Is it dependent on whether I woke up feeling all rotten and angry at myself and the world, winching against the injustice that happens all around me everyday and sometimes involving me directly at my workplace? Or is it my personality that makes me question everything I hear and see, rather than believe it just because it sounds plausible? Bias is inbuilt into humans which constantly suppresses the truth-seeking behaviour that swells up briefly within us when we are supplied information that makes more sense to believe than disbelieve. For example, if someone tells me that 100% of my patients gave me good feedback, I am unquestioningly happy. I had always suspected that anyway. Tell me that 90% of my patients were happy with my care delivery, I am immediately suspicious whether the 10% included that woman who was a hypochondriac and the man who did not have the patience to wait another 10 minutes in clinic. Neither aspects are really feedback on my care, but merely reflection of their own personal traits, I argue. Tell me that only 30% of my patients were happy with my care delivery and I am immediately skeptic of the whole process of the data collection. I am convinced there has been huge bias in patient selection. I am sure that huge throngs of my satisfied patients were never approached for authentic feedback. Now if you tell me that while 90% of my patients were happy with my care, 100% were happy with the care provided by my colleague, I can assure you that is absolutely ridiculous. Now the reliability of the whole process is under question. Let us start with "how did my colleague manage to influence the patient selection"? "Who distributed the questionnaire?" "Were all my patients sick inpatients or demented and confused not to have provided accurate information on my excellent care?" "Did all my patients have prepaid envelopes?" "Were they all literate or was a sizeable proportion intellectually challenged with learning disabilities?" I have always suspected the last one and this survey statistic merely confirms that now! The point is, if your hospital has good statistics on a particular mortality measurement- HSMR, RAMI or SHMI- you choose to believe the statistics that reflect that. There is no reason for a happy London hospital doctor to doubt that the morbid statistics of a desolate hospital in Inverness is untrue. On the other hand, if your own local hospital has a high position on the mortality rate league table, you suspect the veracity of the measurements. So did everyone living near Mid Staffs believe their hospital mortality was true? Probably, because the whole country could not be wrong and there was no data saying otherwise. Did it confirm everyone's suspicions at that time? Probably not. I am sure many were probably happy and grateful for the care that they had received there and kept wondering if they were the exception, the ones that got away without becoming a statistic at that building, where all things evil now lives and breathes like the politicians repeatedly remind us. Yet, where were they till now? The sad truth is that many of us will only fight when our own existence or interests are threatened. Till that breaking point, it is someone else's problem. This happens at all levels of the NHS. Within hospitals or within CCG's the same behaviour will be demonstrable where we wonder why people do not engage with processes trying to improve care. Seemingly good people who have the potential to bring about change do not do the right thing or offer timely solutions but favour inaction and choose to watch from the stands at the unfolding action, as if waiting to see what comes out of it all, as if to see how bad things can get, as if to get personal satisfaction by letting fate prove the "I told you so" clause. I wouldn't go as far as maligning the natural behaviour of vultures and jackals here, but there are undeniable similarities that cannot be ignored. Some people may continue in optimistic expectations, constantly reassuring themselves that it is unlikely to get much worse on their patch, a behaviour not too dissimilar from many of our diabetic patients who sincerely believe that diabetic complications will be other patients' problems and never theirs. When an unexpected turn of events threatens their own existence or jobs or local healthcare sustainability in a mortal fashion, such people may rally to the battle, expressing the views they never expressed, trying to fight the fight they never fought when it could have made a difference. So how can this be addressed. More Berwick reports? More generic training sessions? More mandatory training? More duty of candour clauses? More zero tolerance statements? Printing out Hippocrates Oaths on every remaining space on hospital ward walls? Appointing champions of frankness and truth? Empowering everything that moves to challenge everything that can be challenged? Even more Patient groups/ expert patient groups/LINK groups/ local health watches and hoping some one with a voice turns up for the meeting ? Throw more money to incentivise experienced clinicians to give their erudite opinion in a timely fashion ? Set up groups with fledglings fresh from medical school in the dire hope that some bright spark, however ill-informed, may bring new perspectives to turn things around magically? Give time out for more managers to set out on pilgrimages called "a piece of work" to seek out the hidden truth and answers that they believe exists somewhere out there along with the UFOs? Turn to the centres of apparent excellence -based on this month's statistics-and hope for solutions to be twittered back from greater-than-thou elsewhere? Put the people, who spout goodwill-talk every time they open their mouth, in leadership roles hoping that they can chat people into doing the right thing every time? All that is necessary for the triumph of evil is that good men do nothing is what Edmund Burke said. I say, all that is necessary for the closure of your local hospital is for you to believe everything and do nothing. Blessed are the non-believers for they will continue to have a local hospital. So the Berwick report is now making waves. Peacefully lapping against steadfast rocks. Why peaceful? Because the stress is again on the NO BLAME culture that has to thrive in the NHS for it to be the envy of the world. Business as usual I see.
I would read the Holy Bible usually if I wanted to feel good but now it seems there is another do-gooders' prescription on the block. Generic behaviours wish-list galore for the NHS. Feel good, exhilarating, hair raising feeling of goodness. Help everyone, dont kill your patients, love your neighbouring trust as thyself, forgive even CCG commissioners who denied you money to sustain your services , don't covet another hospital's money and such. A bit different in that there are only 8 commandments. Not exactly called commandments because in this day and age, commandments would be a politically incorrect word. Let us go with "Solutions" instead. If they could call it a guideline, they would but this time solutions turned out to be more popular around the table. I have nothing against this report. To have something against it would make me look pretty much a bad guy who hates a good sermon in church. No, I like it, I like it, I like it. I promise. I enjoy reading it just as much as the next man {or woman, but I am not usually that lucky}. But that does not mean, I cannot see the lighter side of the recommendations. Or should I say, the darker side? Use quantitative targets with caution. Goals in the form of such targets……should never replace the primary goal of better care. In other news, What? Your hospital mortality is 116? It should be at 103! You are not delivering quality care because your quantitative target says otherwise. No, no, dont quote me the berwick report. That report won't run this hospital next year if we don't break even this year. Come on, come on. Solutions please. How many patients should each FY2 clerk in each day? How fast should a registrar respond to a sepsis call? The commissioners want 95.3% of discharge summaries to reach them before 12 midnight if we want our one million pounds. Do you think we could write to them to read solution 5 of the Berwick report? Keep another two copies of the Berwick report to be sent as response to the Monitor next month and the department of health the month after. Ensure that responsibility for functions related to safety and improvement are vested clearly and simply in a thoroughly comprehensible set of agencies, among whom full co-operation is without exception, expected and achieved. I can see the instant response to that statement everywhere in the NHS where people are waiting with open arms to make every paragraph of every report come true. Let us get rid of the current Quality improvement program at our trust and set up another committee named Quality Performance program. While we are at it, we could remove one or two of those clinicians who have been slowing down the quality goodies that have been waiting to be delivered. Or should we call it Quality Innovation productivity and prevention programme? Damn it, all the good ones have been taken. Give it another year, that may become available again. Give the people of the NHS- top to bottom- career long help to learn, master and apply modern methods for quality control, quality improvement and quality planning. I understand control, I understand improvement, I understand planning. What exactly was that "quality" bit thrown in three times in one sentence supposed to do? Would that make that sentence a very high quality statement? People love quality. I do. I ooze it. I know I know, you dont think so? Obviously we haven't met. Anyway, point is, one man's quality is another man's mediocrity. Tell me, when was the last time we rewarded quality? Er, No, that was just numbers, not quality. 20 discharges in a day is not quality. 99.5 % people transferred from one room to another wrong room within four hours is not high quality. 95% of toenail fungal infections seen within 18 weeks and treated is not quality. It would have been of some quality, but the fact that we had no space to fit in the 30% of patients who really needed to be seen urgently with failing hearts because we were busy with the nail fungus made it look a bit silly. Fact is, the people in the NHS who talk about quality are too busy writing or counting, to see the wood for the trees or the quality for the quantity. I realise I am writing as well, I should not be, I know. Make sure that pride and joy in work, not fear, infuse the NHS. Who? Me? Ok, Ok, I will make sure. Er, How? Not in my gift, sorry. I can't mollycoddle those looking and behaving like they know what they are doing but tremble with fear the minute they are called to explain themselves and their mis-behaviour. Oh you poor thing. You saw that the health care assistant switched off the patient's call-button without giving a commode straight away but you did not tell the HCA that it was unacceptable because you were shaking with fear? Or were you trembling with fear at the thought of having to live with a disgruntled HCA(s) ganging up on you for the rest of your life on that ward? Oh Honey, Why did you have to worry? We could have put you into a witness protection programme in an environment free of HCAs for the rest of your life to fearlessly practice nursing the way you always wanted it. Alright then, I see that fear has made you very unsafe. Take the day off tomorrow. There are only 2 nurses for 26 patients tomorrow but take the day off anyway, because your body language tells me you are going to throw a sickie anyway. See you next Wednesday. Please take care not to work in fear. Feel free to take pride in your work from home. When exactly are we going to tell people to take pride and joy in work despite the fear? Good mind-cleansing, sin-dissolving, feel-good talk is fine. But who is going to ensure that EVERY person working in the NHS lives that talk rather than just talk the talk when it suits them? We now live in an NHS environment and training environment where standards have been lowered to get anyone into the workplace and then expect everyone to share the ethos of caring and sharing. There is no more selection happening of committed people. We just hope that being in the shadow of the NHS logo transforms anyone entering, into shining individuals with concern for patients bubbling in their beating hearts. We are also gullible enough, or we choose to be gullible enough to believe that a 46 page document of goodwill will make them contrite, melt their heart and drive them to passionate work on a daily basis. And if it does not turn out that way, please dont blame them. We operate a No blame culture in the NHS. So, Obesity is finally named a disease! The AMA (american medical association) in June 2013 has declared that obesity is a disease state with multiple pathophysiological aspects requiring a range of interventions. For the Americans this has major ramifications with insurers now being forced to cover weight loss therapies ranging from drugs to surgery to behavioural counselling. Doctors' payments also seem to be potentially changed and the obese as well as lean world hold their breath to find out what impact this new classification will have on health service provision in the US.
Obesity is now akin to liver disease and heart attack where all the focus is on how the poor victim will cope with the new onset of the disease and how we as social animals can help them cope with this terrible affliction that God (atheists read Nature) has cursed them with. There are clearly similarities with heart and liver disease that cannot be ignored. A chronic smoker smoking 3 packs a day for the past 20 years gets a heart attack at 45 years of age. Any sympathisers? Oh yes, Other smokers! An alcohol abuser gets cirrhotic liver disease at 35 years of age. Are you empathising with a can of beer in one hand and the mouse in the other? This heart attack and cirrhosis are very similar to those caused by other illnesses as well to a significant degree. Would you treat them like any other heart attack and cirrhosis or would you distinguish between heart-attack-despite-health-lifestyle and heart-attack-of-smoking? Unfortunately No. Is it purely because we cannot tease out the contribution of smoking from other factors causing heart attack in that smoker? Or is it because you are someone who has lived your entire adult life fearing about accusations of discrimination? So how is obesity different you ask. Please see my blog on secondary obesity. Will the AMA distinguish between genetic and lifestyle obesity? Or between obesity due to hypogonadism or that due to emotional overeating? If not, they are doing humanity a grave injustice by legalising food-related highs. Columbians will be clamouring to legalise cocaine next. They may even argue that if food is legal why is cocaine not? Both are addictive and food is even worse in that it probably kills more people worldwide than cocaine. (no reference available, just my suspicion). Currently in the UK, viagra is available for free on the NHS only if the erectile dysfunction is secondary to a disease process like hypogonadism or vascular damage. It has to be paid for if you merely need it to keep your family together. In a similar vein, if the recognition of obesity as a disease crosses the atlantic, would there be patients who would have to pay for obesity treatments versus those who wouldn't have to? I can already hear the shouts of "double standards" and "two-tier system" from the "free-at-the-point-of-care-with-no-questions-asked" brigade. Why is healthcare in Africa poor at diagnosing this disease? Do we need a better and sensitive diagnostic test that can detect this disease in blacks? We have supplied many countries with food and weapons. Suddenly it seems like neither was a good idea after all.... At the end of the day, it is a victory for the obese. They have been absolved of their sins as well as their responsibilities. Millions of poor things have been struck down by the hand of god in their youth. Born with great potential they were stopped from achieving their dreams and aspirations by this deadly life-changing disease that has destroyed their lives and their families' lives. And despite all this suffering, the government has failed them. Lawyers' field day. New nightmare for insurers. But all I am worried about really is what is the obesity SHMI (summary hospital level mortality Indicator) for my hospital going to be next year? OK! it is now official. The NHS is killing people. Although initially set up to save lives, apparently the NHS in the UK is now keen to end life rather than save it. Why else would doctors and nurses in every hospital in the NHS decide to become passionate about transforming into terminators of the elderly and use the now notorious LCP? Not only do they seem to enjoy it, I am told that they even get paid extra to do it. One man's poison is another mans salary?
The usual scare mongering public and the jobless vigilantes have united to put the Liverpool care pathway on its way out. But they are not going to put the LCP on the LCP. They want it to have a painful death. Rubbish it as much as possible. Ten years ago, a ridiculous move as this would have been quelled at the start. Today though, many people are waiting to read more about more failings in the NHS. Not merely because they take pleasure in reading gory stories, but because it gives them a perverse relief that what they suspected deep inside is being confirmed finally! With mortality rates in hospital being projected and framed for everyone to get paranoid about, it was no surprise that the poor LCP took a significant blame for seemingly aiding and abetting the facilitation of high mortality figures. It would not have been a big deal except for the fact that blaming the LCP in effect turns a doctor's compassionate approach into a doctor-death perversity. The very crux of being a doctor is being challenged. It strikes at the very heart of the work ethic of caring professionals who writhe in the frustration of being unable to stand up and fight against these casual allegations which seem to get unfair public support due to the prevailing suspicions of poor care. Yet another sign of the times where we no longer want heroes to shine, but would rather watch villains hurting heroes all along in the movie. We have moved on from the peri-war era where we wanted to hear about good prevailing over evil always. Superman comic strips are now merely looking comical. We want to see him wallowing in kryptonite rather than flying and saving the cat from a tree for a child and looking satisfied. Take away his underwear, make the super S vague and hardly recognisable, and make him look bad by breaking his own oath of never to kill anyone. Yes, I have been to the latest film. Look at all your new Batman movies where villains get more screen time rather than the caped crusader. Toys of villains sell faster. Kids try to pretend to be the Joker with the self inflicted knife wound on the face than be the pathetic caped crusader. Make green lantern gay. Millions have started reading comics now because they can identify with green lantern? Makes one think how we have sold our soul in the search of political correctness and feigned righteousness. I am told they are looking to make superman black. Sorry to diverge, but the point in discussion is not so much about whether LCP is the way forward or not, but instead, how will any dying pathway pretend to be a dying care pathway. Or even more importantly, how can the public be convinced every time that it was not a Lying care pathway? If you are expecting an answer to that, you should stick to the movies above. Like everything in medicine, no one and nothing is infallible, and everyone's actions are open to interpretation, often by vulnerable relatives who get more solace in blaming someone than accepting the inevitable. Any action can be challenged easily, but to stand by and defend one's actions in the face of an angry irrational mob hell bent on blood is the ultimate test of passion and belief in one's actions. If those who have used the LCP dont stand by it, it will be interpreted as admission of guilt. If the merits of the LCP outweigh any potential for abuse in the hands of an occasional shipman, then we should fight against the elbow jerk response of trying to abolish the LCP purely to satisfy a few paranoid people who will continue to fear anything and everything that they do not understand. The LCP may go, because it is un-defendable. Not because it is at fault, but because it is not possible to analyse every case in its clinical real life context to fully satisfy the people shouting for blood. Retrospective reviews of case notes hardly grasp the real state of things where the LCP was instituted. So the LCP will go. But it will be back. But without any credit for Liverpool. That is the way we like it. Why should anyone get any credit. Let us keep it bland. Let us keep things without ownership. We dont want heroes. We just want a normal world where villains get to challenge everything heroes do. You may say that is what makes heroes heroes. I say it makes heroism a dying trait, particularly when the public gets behind the villains. Why is Mortality a problem in the NHS?
A loaded question if I ever have heard one. On one hand, it tends to convey the feeling that mortality is not a problem outside of the NHS. On the other hand, it seems to construe that the NHS is somehow pathologically responsible for every mortality that happens under its kind patronage. "Ageing is a problem in the NHS". Does that convey the inevitability of the problem? Does it make you say, "where is it not"? So why is it that when we talk about the Damocles sword of mortality, we tend to forget the inevitability of the same? Everyday, the public seems keen to prove that doctors are not gods as the doctors seem to think, but when it comes to mortality, they seem to expect doctors to be Gods and avert mortality at every instance? Or is the confusion due to the fact that we casually state "mortality" without qualifying if further? Mortality comes in two forms. "Expected" and "unexpected" mortality with the latter being the one that all of us are concerned about. Yet when it comes to number crunching on the national scene by Dr. Foster or CHKS databases, all this is thrown to the wind and it all comes down to just "mortality" as far as the public is concerned. In the thick of discussions in NHS trusts also this distinction can get easily blurred with loss of focus of what really matters and what really needs to be done. "Needless Deaths". Another trending word for the tabloids and department of health. Yes, I did use them in the same sentence . Attention grabbing is what both of them do as and when they need someone to listen, what else gets the attention of daily mail readers than "needless deaths"?. "Needless " just seems to be a ridiculous word to portray what happened, giving a feeling that there are needed deaths. I won’t go into aspects of euthanasia on this blog! Newspaper flash: "2000 needless deaths might have happened at the Killthemall NHS foundation trust". Might have happened. If that is not scaremongering, I don’t know how you do it better. Coming back to "expected" versus "unexpected" deaths. So apparently there is a mechanism to decide which deaths in hospital are expected. Any event that does not meet the requirement of that risk assessment formula is "unexpected". 99 year old Jones comes into hospital with a cough. Mr. Jones had no expectation of death. Neither did his family who was confident in the NHS's ability (after all NHS does world class commissioning whatever that is, so the care must be world class, better than first class if you ask me)to keep him going forever. They would not have dreamt that he could die suddenly a day after admission. Unexpected Death. What about the Medics who admitted him? They see an old man (don’t accuse me of ageism, just stating the facts as medics see him for the sake of discussion) coming in with the old man's friend, good ol pneumonia with the very high potential for dying on this hospital admission. They don’t want to shock the family out of their optimism and Mr. Jones gets put on room 101a. He dies the next day and doctors take annual leave and scramble for their defence union phone numbers to get help with answering the letters of complaints from well-meaning relatives who appear from all over the world. Works better than Facebook for family reunion. Anyway, staying on track, this has the potential to become national news, with the hospital's outlying mortality rate suddenly coming into heavy scrutiny in the local echo and the daily telegraphs as relatives from Timbuktu pour out their hearts. Just because it was unexpected. What if I told you that Mr. Jones came in with a severe pneumonia renal failure, atrial fibrillation and heart failure and being bedbound due to previous stroke he had no chance of getting past this septicaemia at 99 years of age? Has your expectation changed? If all of this had been explained to the family and the worst outcome prognosticated, would the unexpected become the expected? Root cause analysis and many wasted man hours later, recommendations come out that communication with relatives was the main problem. You didn’t see that coming did you? That was an easy one. Consider Mr. Jones coming in at the penultimate year of potential receipt of the royal birthday card. In the pink of health as Joneses tend to be, enjoying life, living life to the fullest, never been sick in his life, he has a mild cough. Chest infection. Everything looks ok. Chest x-ray ok, ECG ok, Kidney tests and liver tests very reasonable. Next day he dies on ward 101b. Totally unexpected death. Found dead in the morning no less. Outrage. Letters from Timbuktu as before. What do we do? What do medics do? What do trusts do? What do foundation trusts do? What do trusts that already have a high SHMI (Summary hospital-level mortality indicator) do? They don’t have a leg to stand on. Tabloids print the front page news of the unexpected death of a 100 year old man. At the hands of high-earning overpaid NHS doctors again. The following day, the papers get more details on how the poor Mr. Jones was not even offered lifesaving CPR (cardiac resuscitation) as he was found dead in his bed, passing away silently at night, all alone in a dark corner of the monolithic NHS. Our citizens deserve better. They should pass away more slowly on noisy wards after many more blood tests and imaging and a cocktail of the latest antibiotics or chemotherapeutic agents and ideally even a brain transplant if possible. Public expectations. That is what much of this is about. Not about expectations of death, but expectations of the public. But irrespective of the feelings of the relatives and the local news papyrus, the good Mr. Jones may have unwittingly increased the needless death for the hospital on the national scene. Imagine 90 year old Mr. Jones has a cough and stays at home and passes away in his sleep at home. Not too different scenario, except for the bed sheets stamped with NHS logo and the hospital food. (don’t go there, at least not for now). Not worthy of news. Mr. Jones gets a silent funeral for being the greatest father and grandfather of all time and such. Local Hospital SHMI stays low, Relatives save on phone charges from Timbuktu and newspaper columnists hope for war in the middleast to fill their columns tomorrow. The point I have been trying to make was that if a patient dies outside the hospital, the local hospital has a low mortality rate. Simples. A major contributor to SHMI when it comes to unavoidable deaths in frail patients with total expectation of death. Not the only contributor, but the single major contributor in many places. How is your local community working? Is every unwell 100 year old being sent to hospital just because passing away peacefully at home continues to be an unthinkable event? Are all relatives clamouring for hospital admission for all their grand, grand parents because they don’t trust the local GP, PCT or CTP or CCGs's ability to facilitate a peaceful death at home for their relative with terminal cancer? Is every patient with advanced dementia in a nursing home being carted to hospital at the middle of the night just because the bank nurse did not have a clue about what else to do out of hours? Has every institutionalised person or older person had a end of life decision discussed with him or her to avoid unnecessary admission to hospital with all the distress that it entails? Has every person been given a chance to express their end of life wishes to contribute or not contribute to their local hospitals’ naming and shaming ceremony? Forget trying to focus on SHMI numbers till you get those facts right. If you care about your local hospitals staying open, act now! Mortality and staffing levels. Any association you think?
Did you say Yes? Then you are too bright to be working in the NHS. If you said No, you should be working for the department of health. So is there a staffing numbers issue in the NHS? Of course Yes, because that is always the right answer. There has always been and always will be a staffing problem in the NHS. A government organisation of massive proportions with the fourth largest employee list in the world will always have staffing issues. Not because it is unmanageably big and complex, but because it has been managed to death from all sides. Has Virgin, Apple or Microsoft been complaining about staffing issues? Maybe I don’t read tech news column enough, but I suspect you agree with a resounding NO. One more reason to privatise? I wouldn’t blame you if you said yes, but I would be wary of you for the rest of this blog. So where is the staffing issue a problem? In the community? No, GPs run privatised services and one or sometimes a maximum of ten GPs agree that they have enough nurses to click on the computer popups to bring in the QOF monies. No staffing issues there. We don’t want so many nurses. Bye bye dear. Find some other surgery. We will try to see less patients but click more on the patients that we see. After 60% have been clicked on, we don’t need nurses as we will have already achieved the maximum achievable QOF monies. Hard to believe the GPs are part of the NHS. They are contracted for service, with no contract of service. By the people, for the people, but not of the people or something like that. Hospitals on the other hand truly represent the complexity of the benevolent NHS. Enter past the perimeter of the hospital walls and you are in secondary care land. Never land for some. Ever land for others. Point being, these are big organisations trying to stay afloat in the current financial climate, looking towards their neighbours with envy at everything ranging from their PBR rake-in money and SHMI league status to recently conferred foundation status and better recruitment potential due to geographical advantage. It is a dog eat dog world. Not visible on the surface as everyone goes about doing their jobs to their fullest potential, but underneath it all, everyone realises that they are 84th in the league table of shame because of the blessed 83 above them, hospitals strategically placed in enchanted locations, with every junior doctor and nurse, trainee or otherwise, pining to be part of university edifices, trying hard to mingle with the crowds that matter, both at work as well as during the dark pleasurable night life hours in the gay cities nearby. So your local hospital is 145th on the mortality table. Nobody knows how that happened but everyone seems to know that it means that the hospital is dangerous. How do they know? Because the well-meaning politicians of Whitehall have publicised this "death list", to raise awareness among the public about the hideous crimes that go on within hospital grounds up and down the country where sick people are quartered and tortured to death, needlessly. Every day. Even as we speak. And your hospital is 145th on the list. You are told it cant get any lower than that, unless new hospitals are made. There is still hope you say. So you seem to have two options now. One, Register in rightmove and move your family elsewhere to start savouring city life and night clubs like the doctors who chose the bigger cities did and leave your local hospital to perish in shame and let "market forces factor" decide it's future as Virgin and CareUK move in beating their wings, to pick at the cadavers. (I didn’t say vultures, you just conjectured them up). Second option, stay put and ask why your local hospital is performing poorly on the league table and can I stand by it to tell those politicians to get their facts right. I see you chose night life. Low life. Anyway, this is not about you, it is about the hospitals. Focus. There are not enough doctors in the hospital! Would you believe that? We sent 10,000 foreign doctors back just recently (see junior doctors numbers between 2006 and 2007 on the linked excel sheet) because we were apparently in surplus. Some health select committee suggested that that was inappropriate, but you dont have a clue who they are and dont care do you?. So now that we are gaining independence from foreign countries (rather than the other way round as has been historical), and are increasingly recruiting indigenous population to do the job, why are hospitals saying they are not having enough doctors? You still continue to hear about too many consultants, not enough consultant jobs for all the registrars who are coming out, More F1 jobs than CT posts, too many medical students coming out soon..etc. etc., and still hospitals don’t have enough doctors.. But did you know that..... .......EWTD introduction in 2009 has effectively doubled the requirement for doctors' numbers at a time when numbers were already dwindling? ......68,880 nursing jobs have been earmarked to go between April 2010 and April 2015 with 24,836 of these already gone? Forget trying to meet RCN recommendations on safe nursing staffing levels! ......Increasing proportion of female doctors are coming out from medical schools and soon will adopt less than full time working posts, thus doubling requirements further, along with maternity leaves and child care, all requirements of a "compassionate society" which is paradoxically intolerant of the NHS in its current shape and form? ......Recruitment of doctors continues to be a nightmare in district general hospitals that are far away from the glittering cities, and yet offering posts with lower banding thus providing lower salaries, combined with travel money cuts? ..... it is hard for a newly qualified doctor to look after patients well, if half of the junior doctors posts are not filled? Rushed off one's feet while trying to find ones' feet is hardly safe and trying to do two doctor's jobs when you are not even qualified to do one is even more ridiculous. It then seems funny when the government and public keep wondering what the reasons for increasing hospital mortality could be. Staffing issues? You heard it here first. Add injury to this insult. The one doctor who is trying to do the job of two has never worked in the UK before. What is he then doing in the NHS you ask. Well, there was no one else. Someone was needed to be a body in an empty rota. Scant 15-minute long distance telephonic interview later, doctor from non-English speaking country arrives to do a job in a country and a hospital he has never been to before. His only qualification to do the job safely is the 5 minute induction pack handed over to him at the entrance of the hospital with the general direction of the mess room being pointed out by a benevolent health care assistant. Ok, but before you think that the problem is only with the foreign doctors who have come to sort this problem ad hoc, what about educational standards in this country? Tomorrows doctors 1993 document. Life changing for doctors qualifying since, life taking for patients. The beginning of the dumbing down of medical education. Why? Because the new doctor of tomorrow basically only needs to smile and talk sweet little nothings to reassure patients. Knowing the biochemistry and physiology of their bodies was not so crucial. Knowing too much was the problem in the 40 s and 80s. Knowledge makes doctors arrogant. Dumb them down and they are docile and easily manipulated. Doctors in hospitals thought they knew more than those in the community. Solution, dumb down hospital doctors so that they can be moved into the community as required to be whatever role required of them. None of the basics of medical education to be taught anymore! This has been identified as a problem by clinicians (but who listens to them anyway?) and even the backbench MPs of the health select committee highlighted this as a current threat in 2008-2009 report on patient safety (see page 7) . The junior doctor thus qualifying with only communication skills and some pleasantries to get by in daily ward life, hopes to learn most of medicine, post-qualification on the wards. Sadly, she is disillusioned to find that when she is the only doctor in the ward, teaching is unlikely to happen because someone has to rewrite charts and take blood and send blood and give blood as well as leave at the stroke of 5 pm to abide by EWTD regulations. So if anyone asks you what is the cause of increased mortality in the NHS, feel free to boldly say, quantity and quality of nursing and medical staff. But word of caution: Ask them for solutions before they ask you..... |
AuthorLuxy John Warning!May contain Nuts, Sarcasm and cynicism.
DisclaimerThe content of the blogs is not representative of my views about my local hospital or CCG, but instead is based on the generic issues in the wider NHS landscape.
Archives
May 2017
Categories
All
|
 RSS Feed
RSS Feed