Hypertension, dyslipidaemia, hyperglycaemia, and smoking do not totally account for the cardiovascular events associated with obesity. In recent times, a pro-thrombotic state involving disturbances in the haemostatic and fibrinolytic pathways are being increasingly recognised as contributing to the excess cardiovascular risk in obesity. The disturbances in this coagulation pathways include platelet hyper-aggregability (increased Von-Williebrand factor), hypercoagulability (increased fibrinogen, factor VII, and factor VIII), and hypofibrinolysis (increased plasminogen activator inhibitor PAI-1 levels) . Fibrinolysis is normally mediated by plasmin, which circulates in blood as its pro-enzyme, plasminogen. Conversion and activation of plasminogen into plasmin is effected by two plasminogen activators; Tissue type plasminogen activator (t-PA) and Urokinase type plasminogen activator (u-PA). Baillieres Clin Haematol. 1995 Jun;8(2):277-90 The process of fibrinolysis can thus be inhibited by inhibition plasmin itself by α-2 anti-plasmin, or by inhibition of the plasminogen activators by PAI-1.
PAI-1 production and distribution
PAI-1 is a serine protease inhibitor that inhibits fibrinolysis by inactivating urokinase-type and tissue-type plasminogen activator. PAI-1 is also involved in angiogenesis and atherogenesis. PAI-1 is normally secreted by endothelial cells, vascular smooth muscle cells, hepatocytes platelets and the Adipocytes. Diabete Metab. 1991 May;17(1 Pt 2):96-100 Majority of the circulating PAI-1 is contributed to by adipose tissue. Obes Rev. 2002 May;3(2):85-101. Thus obese subjects have higher levels of PAI-1. Int J Obes Relat Metab Disord. 1997 Jul;21(7):527-535. In fact, BMI has been shown to correlate with PAI-1 levels irrespective of gender and age. Metabolism. 1986 Mar;35(3):250-3. Arterioscler Thromb Vasc Biol. 1998 Apr;18(4):562-7 Visceral adipose tissue secretes more PAI-1 than subcutaneous adipose tissue, Nat Med. 1996 Jul;2(7):800-3. Endocr Rev. 2000 Dec;21(6):697-738 and in keeping with this, Waist Hip ration (WHR) has been shown to correlate with PAI-1 levels. Metabolism. 1990 Oct;39(10):1044-8. Plasma levels of PAI-1 correlate with visceral adiposity independent of insulin sensitivity, Arterioscler Thromb Vasc Biol. 1998 Nov;18(11):1716-22 and triglyceride levels. Am J Clin Nutr. 1998 Jun;67(6):1136-40. Interestingly, omental (visceral) as well as subcutaneous fat in the obese show higher expression of PAI-1 compared to non-obese subjects. Diabetologia. 1998 Jan;41(1):65-71. Normally, subcutaneous fat is more in amount than visceral fat. Subcutaneous fat also produces PAI-1 and hence most of the PAI-1 in non-obese subjects is produced from subcutaneous fat, with increasing contribution from visceral adipose tissue with central weight gain. Studies have shown variable results in the contribution of subcutaneous vs. visceral fat towards PAI-1 in obese individuals. Thromb Haemost. 2000 Apr;83(4):545-8.; Diabetes. 2000 Aug;49(8):1374-80.
PAI-1 and cardiovascular disease
PAI-1 levels can predict future risk for type2 diabetes and cardiovascular disease. A lowered fibrinolytic state Lancet. 1993 Oct 30;342(8879):1076-9. as well as an increased plasma PAI-1 activity Lancet. 1987 Jul 4;2(8549):3-9. ; Arterioscler Thromb Vasc Biol. 2000 Aug;20(8):2019-23. have both been shown to be independently associated with increased risk of future CHD events or recurrent events respectively. High levels of plasma PAI-1 activity was also shown to be associated with a higher risk for first Myocardial infarction in prospective studies on healthy individuals. Circulation. 1998 Nov 24;98(21):2241-7 But, not all studies have shown a correlation between PAI-1 levels and cardiovascular events. Br Heart J. 1991 Nov;66(5):351-5. ; Circulation. 1993 Nov;88(5 Pt 1):2030-4. In fact, tissue plasminogen levels (t-PA) levels were more likely to be correlated with cardiovascular events than PAI-1 levels. N Engl J Med. 1995 Mar 9;332(10):635-41 ; Thromb Haemost. 1998 Jan;79(1):129-33; Lancet. 1993 May 8;341(8854):1165-8.
PAI-1 modulators
Plasma PAI-1 activity is highest between 12 midnight and 6 am. Thromb Haemost. 1988 Apr 8;59(2):329-32 Age related changes in PAI-1 have not been consistent in studies. Younger men have higher PAI-1 than women. Arterioscler Thromb Vasc Biol. 1998 Apr;18(4):562-7, while postmenopausal women have higher plasma PAI-1 than pre-menopausal women. Circulation. 1995 Apr 1;91(7):1952-8. HRT therapy seems to be associated with lower PAI-1 levels in postmenopausal women. Am J Epidemiol. 1996 Jan 15;143(2):159-66. PAI-1 levels correlate negatively with Testosterone levels. Metabolism. 1989 Oct;38(10):1010-5. Plasma levels of PAI-1 correlate positively with features of the metabolic syndrome. PAI-1 levels are higher in obesity and insulin resistance. Levels of PAI-1 fall after weight loss induced by thiazolidinediones. Alcohol intake and smoking increase PAI-1 levels. Thromb Haemost. 1998 Nov;80(5):749-56.
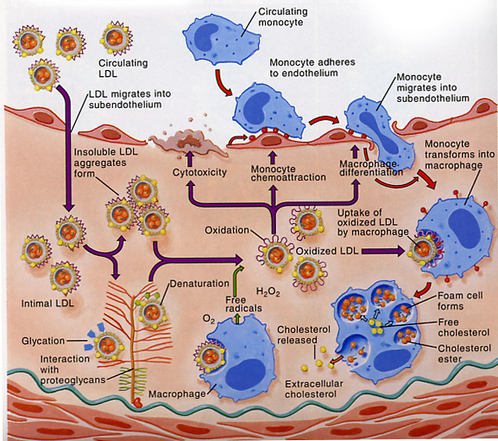
PAI-1 production is increased by TNF-α, Atherosclerosis. 1999 Mar;143(1):81-90. Angiotensin II, Interleukin-1β, Arterioscler Thromb Vasc Biol. 2000 Jun;20(6):1682-7. TGF-β, Diabetes. 2000 Aug;49(8):1374-80 glucocorticoids, Diabetes. 1999 Apr;48(4):890-5 and insulin J Clin Endocrinol Metab. 1999 Nov;84(11):4097-105 while PAI-1 expression and secretion by adipocytes is decreased by catecholamines. J Clin Endocrinol Metab. 1999 Nov;84(11):4097-105 Regulation of PAI-1 acutely by insulin seems unlikely, Thromb Haemost. 1991 Feb 12;65(2):130-3. while studies have suggested that chronic hyperinsulinism in obese diabetic patients may explain the raised expression of PAI-1 in adipose tissue. Diabetes Metab Res Rev. 2000 Sep-Oct;16(5):364-9. TNF α which is also produced by adipocytes, may through its stimulatory effects on PAI-1, mediate the production of insulin resistance. TNF α-stimulated PAI-1 secretion is decreased dose-dependently by thiazolidinediones (troglitazone and pioglitazone), Biochem Biophys Res Commun. 1999 May 10;258(2):431-5. suggesting a role for PPAR γ in the regulation of PAI-1. Anti TNF-α treatment produces a fall in production and levels of PAI-1. Obes Rev. 2002 May;3(2):85-101. Leptin levels are positively correlated with PAI-1 plasma levels and activity independently of insulin and fat mass, although a regulatory effect remains to be clarified. Metabolism. 1999 Aug;48(8):960-4. VLDL and Lipoprotein (a), Arterioscler Thromb Vasc Biol. 1997 Nov;17(11):3215-23. as well as oxidised LDL Arterioscler Thromb. 1991 Nov-Dec;11(6):1821-9. all of which are implicated in the insulin resistance syndrome, have all been shown to increase endothelial production of PAI-1. Lipoprotein (a) a specialised form of LDL, through its structural similarity to plasminogen, interferes with fibrinolysis by competing with plasminogen binding to plasminogen receptors, fibrinogen and fibrin, resulting in impaired plasminogen activation and plasmin generation. Arteriosclerosis. 1990 Mar-Apr;10(2):240-5.
A 24 hour fast decreases PAI-1 activity, Metabolism. 1986 Mar;35(3):250-3. as does weight loss Metabolism. 1995 May;44(5):611-6. and treatment with metforminMetabolism. 1997 Apr;46(4):454-7. or thiazolidinediones. Diabetes. 2000 Apr;49(4):633-9. While <10% weight loss decreases PAI-1 levels by up to 55%, Arterioscler Thromb. 1993 Feb;13(2):162-9. >10% weight loss is associated with as much as 70% reduction in PAI-1 levels irrespective of the method of weight loss production. Thromb Haemost. 1992 Oct 5;68(4):396-9, Arterioscler Thromb Vasc Biol. 1999 Jun;19(6):1582-7 , Eur J Clin Nutr. 1998 May;52(5):329-33, Despite the consistently strong suggestion that weight loss produces a reduction in PAI-1 levels, it is still not clear whether the reduction is related to visceral adipose tissue loss itself Int J Obes Relat Metab Disord. 1998 Apr;22(4):312-7. Thromb Haemost. 1999 Nov;82(5):1490-6. or due to changes in metabolic factors as triglycerides Eur J Clin Nutr. 1998 May;52(5):329-33, Am J Clin Nutr. 1996 Jul;64(1):7-11; Arterioscler Thromb Vasc Biol. 1999 Jun;19(6):1582-7
Mice lacking PAI-1 show decreased weight gain despite a high fat diet with increased energy expenditure, improved glucose tolerance and enhanced insulin sensitivity.Diabetes. 2004 Feb;53(2):336-46 Deletion of PAI-1 in the ob/ob mouse decreases adiposity. FASEB J. 2001 Aug;15(10):1840-2 Polymorphisms of the PAI-1 gene have been described, but despite some studies showing an association with cardiac events, Thromb Haemost. 1998 Dec;80(6):1029-30; Arterioscler Thromb Vasc Biol. 1997 Jan;17(1):33-7 their impact on cardiovascular risk remains to be defined.
PAI-1 production and distribution
PAI-1 is a serine protease inhibitor that inhibits fibrinolysis by inactivating urokinase-type and tissue-type plasminogen activator. PAI-1 is also involved in angiogenesis and atherogenesis. PAI-1 is normally secreted by endothelial cells, vascular smooth muscle cells, hepatocytes platelets and the Adipocytes. Diabete Metab. 1991 May;17(1 Pt 2):96-100 Majority of the circulating PAI-1 is contributed to by adipose tissue. Obes Rev. 2002 May;3(2):85-101. Thus obese subjects have higher levels of PAI-1. Int J Obes Relat Metab Disord. 1997 Jul;21(7):527-535. In fact, BMI has been shown to correlate with PAI-1 levels irrespective of gender and age. Metabolism. 1986 Mar;35(3):250-3. Arterioscler Thromb Vasc Biol. 1998 Apr;18(4):562-7 Visceral adipose tissue secretes more PAI-1 than subcutaneous adipose tissue, Nat Med. 1996 Jul;2(7):800-3. Endocr Rev. 2000 Dec;21(6):697-738 and in keeping with this, Waist Hip ration (WHR) has been shown to correlate with PAI-1 levels. Metabolism. 1990 Oct;39(10):1044-8. Plasma levels of PAI-1 correlate with visceral adiposity independent of insulin sensitivity, Arterioscler Thromb Vasc Biol. 1998 Nov;18(11):1716-22 and triglyceride levels. Am J Clin Nutr. 1998 Jun;67(6):1136-40. Interestingly, omental (visceral) as well as subcutaneous fat in the obese show higher expression of PAI-1 compared to non-obese subjects. Diabetologia. 1998 Jan;41(1):65-71. Normally, subcutaneous fat is more in amount than visceral fat. Subcutaneous fat also produces PAI-1 and hence most of the PAI-1 in non-obese subjects is produced from subcutaneous fat, with increasing contribution from visceral adipose tissue with central weight gain. Studies have shown variable results in the contribution of subcutaneous vs. visceral fat towards PAI-1 in obese individuals. Thromb Haemost. 2000 Apr;83(4):545-8.; Diabetes. 2000 Aug;49(8):1374-80.
PAI-1 and cardiovascular disease
PAI-1 levels can predict future risk for type2 diabetes and cardiovascular disease. A lowered fibrinolytic state Lancet. 1993 Oct 30;342(8879):1076-9. as well as an increased plasma PAI-1 activity Lancet. 1987 Jul 4;2(8549):3-9. ; Arterioscler Thromb Vasc Biol. 2000 Aug;20(8):2019-23. have both been shown to be independently associated with increased risk of future CHD events or recurrent events respectively. High levels of plasma PAI-1 activity was also shown to be associated with a higher risk for first Myocardial infarction in prospective studies on healthy individuals. Circulation. 1998 Nov 24;98(21):2241-7 But, not all studies have shown a correlation between PAI-1 levels and cardiovascular events. Br Heart J. 1991 Nov;66(5):351-5. ; Circulation. 1993 Nov;88(5 Pt 1):2030-4. In fact, tissue plasminogen levels (t-PA) levels were more likely to be correlated with cardiovascular events than PAI-1 levels. N Engl J Med. 1995 Mar 9;332(10):635-41 ; Thromb Haemost. 1998 Jan;79(1):129-33; Lancet. 1993 May 8;341(8854):1165-8.
PAI-1 modulators
Plasma PAI-1 activity is highest between 12 midnight and 6 am. Thromb Haemost. 1988 Apr 8;59(2):329-32 Age related changes in PAI-1 have not been consistent in studies. Younger men have higher PAI-1 than women. Arterioscler Thromb Vasc Biol. 1998 Apr;18(4):562-7, while postmenopausal women have higher plasma PAI-1 than pre-menopausal women. Circulation. 1995 Apr 1;91(7):1952-8. HRT therapy seems to be associated with lower PAI-1 levels in postmenopausal women. Am J Epidemiol. 1996 Jan 15;143(2):159-66. PAI-1 levels correlate negatively with Testosterone levels. Metabolism. 1989 Oct;38(10):1010-5. Plasma levels of PAI-1 correlate positively with features of the metabolic syndrome. PAI-1 levels are higher in obesity and insulin resistance. Levels of PAI-1 fall after weight loss induced by thiazolidinediones. Alcohol intake and smoking increase PAI-1 levels. Thromb Haemost. 1998 Nov;80(5):749-56.
PAI-1 production is increased by TNF-α, Atherosclerosis. 1999 Mar;143(1):81-90. Angiotensin II, Interleukin-1β, Arterioscler Thromb Vasc Biol. 2000 Jun;20(6):1682-7. TGF-β, Diabetes. 2000 Aug;49(8):1374-80 glucocorticoids, Diabetes. 1999 Apr;48(4):890-5 and insulin J Clin Endocrinol Metab. 1999 Nov;84(11):4097-105 while PAI-1 expression and secretion by adipocytes is decreased by catecholamines. J Clin Endocrinol Metab. 1999 Nov;84(11):4097-105 Regulation of PAI-1 acutely by insulin seems unlikely, Thromb Haemost. 1991 Feb 12;65(2):130-3. while studies have suggested that chronic hyperinsulinism in obese diabetic patients may explain the raised expression of PAI-1 in adipose tissue. Diabetes Metab Res Rev. 2000 Sep-Oct;16(5):364-9. TNF α which is also produced by adipocytes, may through its stimulatory effects on PAI-1, mediate the production of insulin resistance. TNF α-stimulated PAI-1 secretion is decreased dose-dependently by thiazolidinediones (troglitazone and pioglitazone), Biochem Biophys Res Commun. 1999 May 10;258(2):431-5. suggesting a role for PPAR γ in the regulation of PAI-1. Anti TNF-α treatment produces a fall in production and levels of PAI-1. Obes Rev. 2002 May;3(2):85-101. Leptin levels are positively correlated with PAI-1 plasma levels and activity independently of insulin and fat mass, although a regulatory effect remains to be clarified. Metabolism. 1999 Aug;48(8):960-4. VLDL and Lipoprotein (a), Arterioscler Thromb Vasc Biol. 1997 Nov;17(11):3215-23. as well as oxidised LDL Arterioscler Thromb. 1991 Nov-Dec;11(6):1821-9. all of which are implicated in the insulin resistance syndrome, have all been shown to increase endothelial production of PAI-1. Lipoprotein (a) a specialised form of LDL, through its structural similarity to plasminogen, interferes with fibrinolysis by competing with plasminogen binding to plasminogen receptors, fibrinogen and fibrin, resulting in impaired plasminogen activation and plasmin generation. Arteriosclerosis. 1990 Mar-Apr;10(2):240-5.
A 24 hour fast decreases PAI-1 activity, Metabolism. 1986 Mar;35(3):250-3. as does weight loss Metabolism. 1995 May;44(5):611-6. and treatment with metforminMetabolism. 1997 Apr;46(4):454-7. or thiazolidinediones. Diabetes. 2000 Apr;49(4):633-9. While <10% weight loss decreases PAI-1 levels by up to 55%, Arterioscler Thromb. 1993 Feb;13(2):162-9. >10% weight loss is associated with as much as 70% reduction in PAI-1 levels irrespective of the method of weight loss production. Thromb Haemost. 1992 Oct 5;68(4):396-9, Arterioscler Thromb Vasc Biol. 1999 Jun;19(6):1582-7 , Eur J Clin Nutr. 1998 May;52(5):329-33, Despite the consistently strong suggestion that weight loss produces a reduction in PAI-1 levels, it is still not clear whether the reduction is related to visceral adipose tissue loss itself Int J Obes Relat Metab Disord. 1998 Apr;22(4):312-7. Thromb Haemost. 1999 Nov;82(5):1490-6. or due to changes in metabolic factors as triglycerides Eur J Clin Nutr. 1998 May;52(5):329-33, Am J Clin Nutr. 1996 Jul;64(1):7-11; Arterioscler Thromb Vasc Biol. 1999 Jun;19(6):1582-7
Mice lacking PAI-1 show decreased weight gain despite a high fat diet with increased energy expenditure, improved glucose tolerance and enhanced insulin sensitivity.Diabetes. 2004 Feb;53(2):336-46 Deletion of PAI-1 in the ob/ob mouse decreases adiposity. FASEB J. 2001 Aug;15(10):1840-2 Polymorphisms of the PAI-1 gene have been described, but despite some studies showing an association with cardiac events, Thromb Haemost. 1998 Dec;80(6):1029-30; Arterioscler Thromb Vasc Biol. 1997 Jan;17(1):33-7 their impact on cardiovascular risk remains to be defined.